What Is Vulvitis?
 Vulvitis is a gynecological condition in which the external female genitalia, called the vulva, becomes inflamed. Vulvitis can affect women of all ages and backgrounds. It disrupts your ability to engage in daily tasks and maintain intimate relationships. It also has serious long-term risks if left untreated, including permanent genital scarring.
Vulvitis is a gynecological condition in which the external female genitalia, called the vulva, becomes inflamed. Vulvitis can affect women of all ages and backgrounds. It disrupts your ability to engage in daily tasks and maintain intimate relationships. It also has serious long-term risks if left untreated, including permanent genital scarring.
At Cohen Medical Practice (CMP) in Midtown New York City, you have a team of experienced gynecologists who understand effective treatment options for vulvitis. Dr. Felix Cohen and his team are committed to using their state-of-the-art facilities to provide accurate diagnosis and treatment for a wide range of feminine health conditions. You get a personalized treatment plan and advice to get back to optimal health.
Why Do I Have Vulvitis?
Various triggers can lead to vulvitis including irritants, allergies and infections. You’re more at risk if you have a history of gynecological infections like herpes and yeast infections. Certain products like harsh soaps and douches can also irritate the vulva.
Some people experience vulvitis because of hormonal changes, especially during menopause or pregnancy.
Some of the most common vulvitis triggers include:
- Skin conditions that cause inflammation and irritation, such as eczema and psoriasis
- Allergic reactions to products like latex and spermicides
- Poor hygiene, especially improper wiping
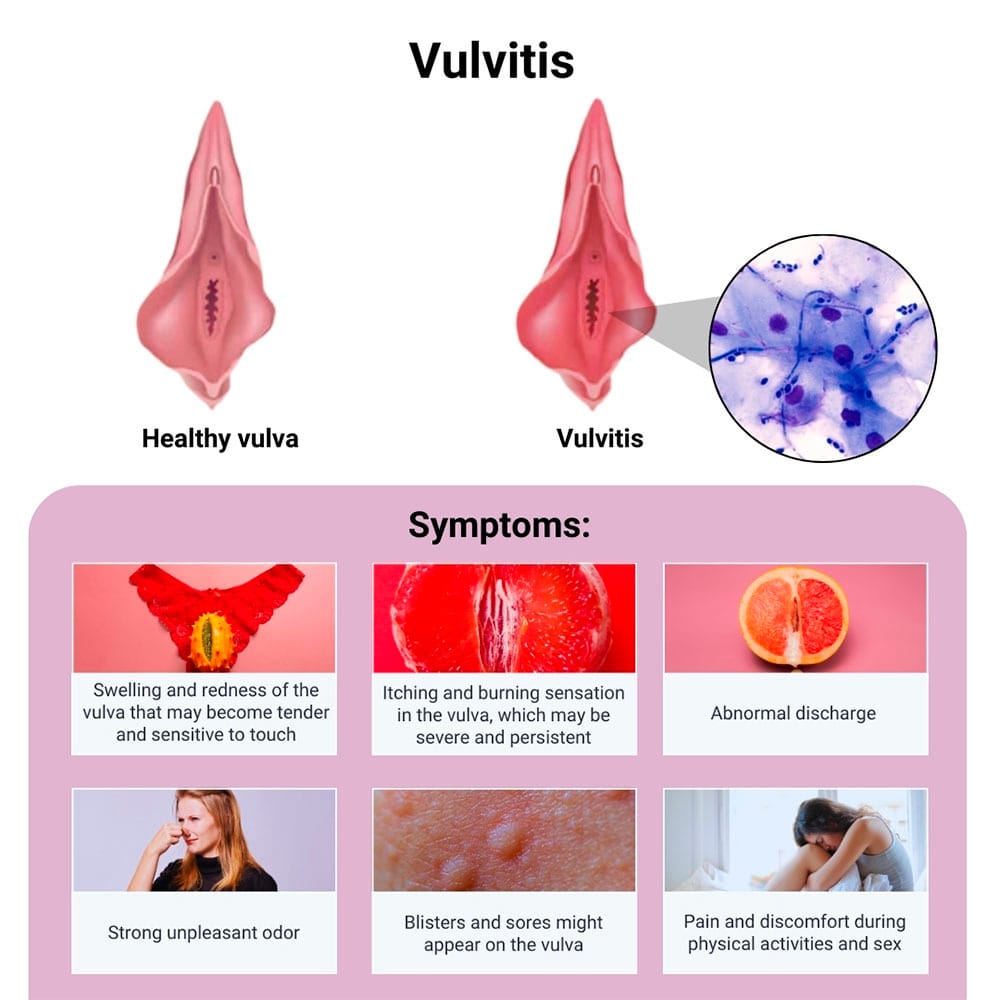
What Are the Signs of Vulvitis?
Different vulvitis symptoms may appear suddenly or gradually. You may experience these symptoms within a few hours or days after exposure to a trigger. These signs of inflammation sometimes resolve on their own. At other times, they persist because the underlying cause continues to go untreated.
Vulvitis symptoms are also often seen in other conditions, such as vaginitis.
However, differentiating symptoms include:
- Swelling and redness of the vulva that may become tender and sensitive to touch
- Itching and burning sensation in the vulva, which may be severe and persistent
- Abnormal discharge
- Strong unpleasant odor
- Blisters and sores might appear on the vulva
- Pain and discomfort during physical activities and sex
How Do I Know if I Have Vulvitis?
Vulvitis is sometimes challenging to diagnose because it shares symptoms with other conditions, especially vaginitis. Both conditions cause abnormal discharge and itching, but vulvitis affects the vulva, whereas vaginitis is a condition affecting the vagina.
The gynecologists at CMP New York have several procedures and tests at hand to diagnose vulvitis accurately.
You might undergo procedures and tests such as:
- Physical gynecological exam to check for inflammation and infection, providing your doctor with a clear path to a definitive diagnosis
- Vaginal swab to examine for infection
- Urinalysis to examine the characteristics and contents of the urine
- Allergy test for different allergens to identify those triggering an allergic reaction
What Are the Risks of Untreated Vulvitis?
Untreated vulvitis can lead to more complex problems with significant health implications and impact on your quality of life. It causes chronic inflammation, scarring and tissue damage that might be irreversible.
The persistent swelling also leads to chronic pain and discomfort that can’t be relieved. Even walking becomes unbearable.
The risks of untreated vulvitis include:
- Adhesions and scarring in the vulva and vagina causing painful sex
- Vaginal narrowing that also causes painful sex
Higher risks of secondary infections such as urinary tract infections (UTIs) and pelvic inflammatory disease. Emotional distress and depression from persistent pain and the negative impact it makes on your daily life
What Are the Most Effective Treatments for Vulvitis?
Your CMP gynecologist determines the most effective treatment depending on the underlying condition. He uses the best combination of treatments to address discomforting symptoms while also advising you on how to treat the underlying cause.
CMP New York has a personalized treatment plan for each case, ensuring alleviation of symptoms and prevention of more complicated conditions.
Some of the treatment options available include:
- Antibiotics to take care of bacterial sexually transmitted infections like trichomoniasis and bacterial vaginosis
- Antifungals to combat fungal growth in yeast infections
- Topical creams like hydrocortisone to reduce inflammation and itching
- Pain relief medications, which usually consist of over-the-counter pain relievers to ease discomfort
How Can I Avoid a Vulvitis Recurrence?
The best way to avoid the recurrence of vulvitis is to make lifestyle and behavioral changes. Your gynecologist advises which adjustments you need to make even as the treatment is ongoing, as well as after you complete the medication.
One of the most effective adjustments is observing proper genital hygiene, especially wiping properly after using the toilet.
Other tips your gynecologist recommends include:
- Avoiding known irritants and allergens such as scented soaps and douches
- Wearing breathable clothing to prevent bacterial and fungal growth
- Maintaining a healthy diet to promote body immunity
- Getting regular gynecological check-ups to detect problems early
Vulvitis is a manageable condition and effectively treatable with the right medical and lifestyle interventions. Although it’s not life-threatening, it’s essential to seek medical attention quickly to avoid more serious complications and damage.
CMP is a trusted medical provider to treat and manage vulvitis and other feminine health problems. Their knowledge, experience and state-of-the-art facilities enable the best possible care. Contact Cohen Medical Practice (CMP) today to take the first step toward healing and wellness.

