What Is Dyspareunia?
Persistent or recurring pain during sex or pain after sex is known as dyspareunia. As many as one in five women or those assigned female at birth experience vaginal pain or pelvic pain after or during sex. Besides physical discomfort, dyspareunia can have a negative impact emotionally and it may affect the intimacy of a relationship.
Pain related to intercourse can be hard to talk about because it’s a sensitive subject, but when sex hurts or your vagina burns after sex, it’s time to reach out to an expert in the field of gynecological medicine. You’ll find a compassionate and experienced listener in Dr. Felix Cohen at Cohen Medical Practice (CMP). He pinpoints the cause of your internal vaginal pain and recommends the most effective treatment to obtain relief.
What Are the Symptoms of Dyspareunia?
The way the discomfort of dyspareunia is experienced can vary from one woman to another.
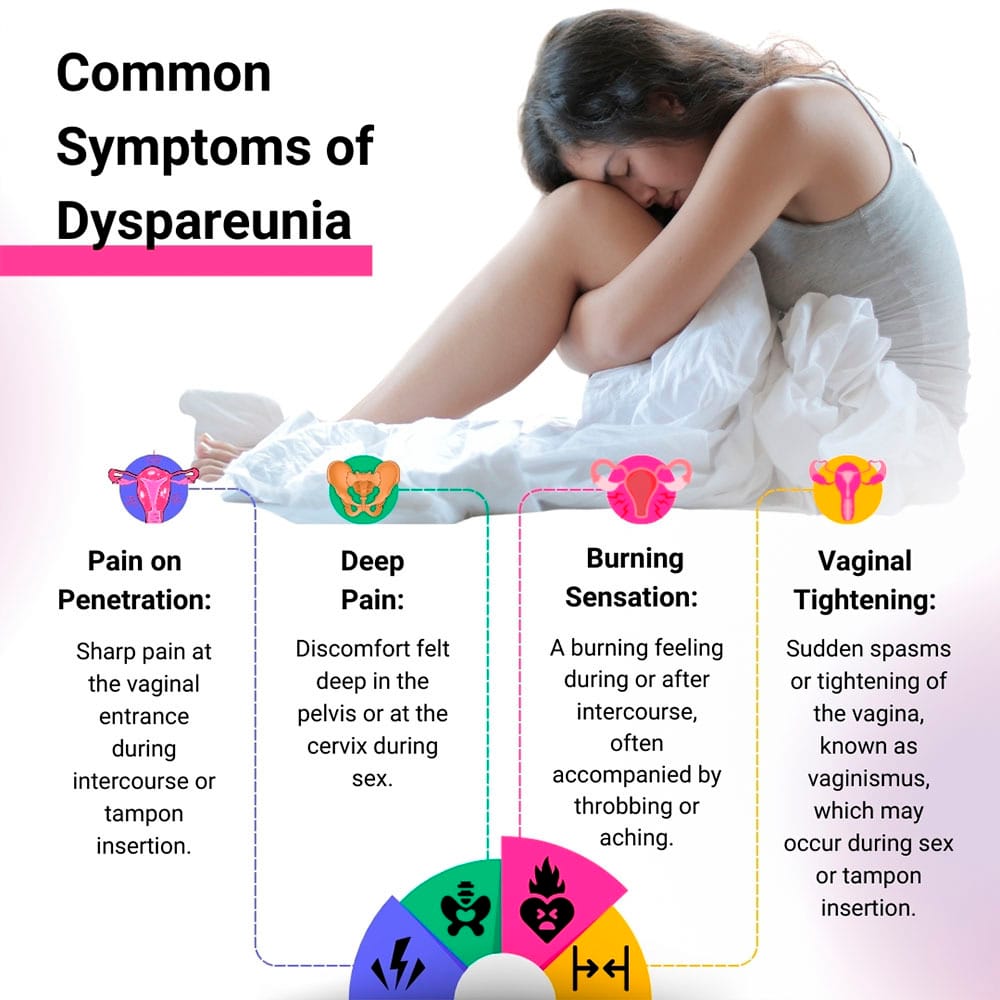
However, the most common symptoms of dyspareunia include:
- Pain on penetration. You may experience sharp pain at the entrance of the vagina from intercourse or from inserting a tampon.
- Deep pain. Cervix pain during sex is an example of dyspareunia that’s experienced as pain deep in the pelvis or internal vaginal pain.
- Burning. Some women experience burning after sex or during sex. Throbbing or aching may continue after intercourse.
- Vaginal tightening. If the vagina suddenly spasms or tightens during sex, it’s known as vaginismus. Spasms may also be triggered by tampon insertion or a gynecological exam.
Women with dyspareunia can feel pain in just one area anywhere in the pelvic region, or pain may be felt in the back, the bladder or the entire genital area. Pain may be experienced as soon as you become sexually active, or it may develop after previously having pain-free sex. If you have dyspareunia, you may find sex painful only at certain times, or every time you have sex.
What Causes Dyspareunia?
There are many possible causes of dyspareunia starting with lack of sufficient vaginal lubrication. Dryness can be a side effect of certain medications such as antihistamines.
Other possible causes include:
- Injury or trauma. Injury from an accident, female genital mutilation, childbirth or from prior surgeries can cause vaginal pain.
- Infection or irritation. Many types of infection can cause discomfort or burning from sex, such as urinary tract infections, vaginal yeast infections or sexually transmitted diseases. Infection that affects one or more of the upper reproductive organs is called pelvic inflammatory disease.
- Irritation. Genital irritation can be caused by a variety of things such as an allergic reaction to spermicides, soap or clothing.
- Endometriosis. This is a condition in which tissue like the lining of the uterus grows in other areas, which can be very painful.
- Fibroids. Pelvic pain, including pain during or after sex, can be caused by non-cancerous growths in the uterus called fibroids.
- Menopause. Decreasing levels of estrogen during perimenopause and menopause can cause vaginal dryness. Postmenopausal women frequently experience thinning of the vaginal lining, making it even more sensitive.
Intercourse can be painful or uncomfortable after childbirth. Emotional factors such as a history of sexual abuse can cause pelvic muscles to tighten leading to discomfort or pain. Lack of arousal, relationship problems or fear of intimacy can also affect whether you’re able to enjoy sex without discomfort.
What Are the Treatment Options for Dyspareunia?
Obtaining relief from dyspareunia depends on identifying the cause. To diagnose dyspareunia and to pinpoint the cause, your CMP gynecologist does a thorough medical history, an abdominal exam and a pelvic exam to check for abnormalities and sensitivity. Additional tests may be ordered such as a pelvic ultrasound.
Treatment for dyspareunia may include:
- Medication may be prescribed such as antibiotics or antifungal medications to treat bacterial infections or yeast infections.
- Estrogen creams, rings or tablets relieve vaginal dryness from menopause.
- Physical therapy may be recommended for pelvic floor dysfunction.
- Injections of corticosteroids can relieve pain following childbirth or vaginal surgery.
- Surgery may be recommended to remove abnormal tissue growth if pain is caused by endometriosis.
Your doctor also may recommend various lifestyle, at-home remedies to relieve the pain or burning you experience during or after sex, such as:
- Using a water or silicone-based lubricant to help relieve vaginal dryness
- Taking an over-the-counter pain medication before sex
- Avoiding fragranced toilet paper, wipes or scented sanitary napkins
- Soaking in a warm bath after intercourse
- Applying ice or a frozen gel pack to your genitals after sex
If you have frequent pain during or after sex, see an expert in the field of obstetrics and gynecology. When you’re looking for a Midtown NYC gynecology practice, look no further than the board certified physicians at Cohen Medical Practice (CMP). Contact your New York City gynecologist if you have abnormal vaginal discharge, irregular periods, genital lesions or any other symptoms that concern you.

