What Is Urinary Incontinence and Its Symptoms?
Urinary incontinence refers to being unable to store or voluntarily control urination. The level of incontinence may be minor, such as leaking or being unable to retain urine, but it’s always bothersome. While anyone can suffer from various types of incontinence, the condition is more common in women as you age, as well as during pregnancy and menopause.
Urinary incontinence may be temporary or chronic, depending on the cause and the severity and often results in withdrawal from social activities to avoid embarrassing situations. It also can cause urinary tract Infections if not appropriately treated.
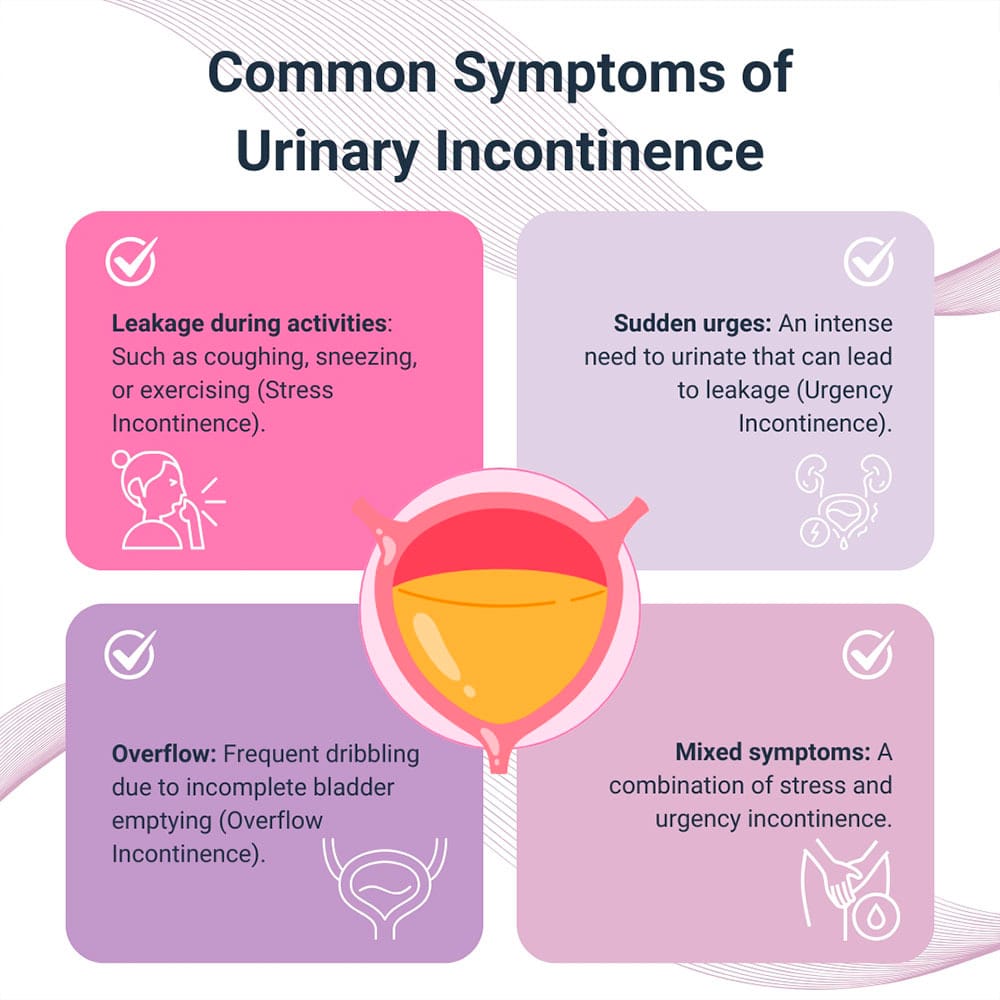
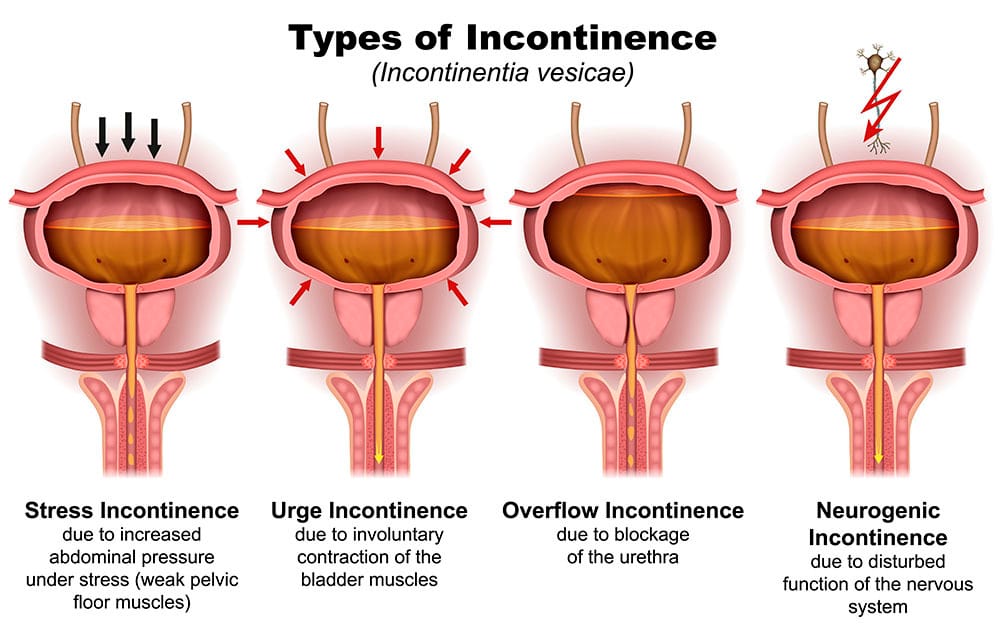
Types of incontinence include:
- Stress incontinence. This occurs when pressure from physical activities leads to urine leakage.
- Urgency incontinence. This refers to a persistent urgent need to urinate, potentially leading to interstitial cystitis.
- Overflow incontinence. Overflow happens when you experience spillage following voiding.
- Mixed incontinence. This is both a combination of stress and urge incontinence, having symptoms of each type.
Incontinence is a treatable problem when you have an experienced doctor who recognizes the signs. Dr. Felix Cohen and his team at Cohen Medical Practice (CMP) in Midtown NYC is a board certified obstetrician and gynecologist and your number one go-to doctor for reproductive problems and all your gynecological needs, from PMS to menopause.
What Causes Urinary Incontinence in Women?
The causes of urinary incontinence are associated with changes to the body that reduce the muscle mass or nerves associated with your bladder control. These could be life-event-related conditions like pregnancy, child delivery and aging or caused by disease or lifestyle factors. When the cause is realized, then your CMP New York physician selects the best form of treatment.
Common causes include:
- Pregnancy and child delivery, due to pressure of the fetus during pregnancy as well as damages that may have been caused during vaginal delivery
- Menopause, when the urethra and bladder muscles are weakened
- Obesity that increases bladder pressure
- Ovarian cysts that can press on the bladder and make control difficult
- Smoking, which leads to a chronic cough that stresses pelvic floor muscles, potentially leading to PCOS
- Diet, especially when it consists of bladder irritants like caffeine, alcohol and spicy foods
- Lack of exercise, which leads to weak pelvic floor muscles that reduce bladder control and may even cause pelvic prolapse
- Diabetes, which can damage the nerves that control the bladder
Neurological conditions such as multiple sclerosis, stroke, spinal injuries, Parkinson’s disease and brain tumors can disrupt nerve passageways used for bladder control, leading to a neurogenic bladder, when your bladder nerves and muscles don’t cooperate with brain communication. Bladder endometriosis is a rare form of incontinence that causes pain when your bladder is full and requires an experienced diagnostician to uncover.
How Is Urinary Incontinence Diagnosed?
Diagnosis of incontinence follows a thorough examination. Your NYC doctor asks about your symptoms, lifestyle and other factors that may be bringing on the types of incontinence.
Proper diagnosis ensures proper treatment and may include other forms of diagnosis, such as:
- Bladder diary. You’re asked to keep a chart of the frequency of urination, the amount and the time of leakage.
- Urinalysis. This requires multiple urine samples for comparison purposes.
- Post-void residual measurement. This is a test that measures urine left in the bladder post urination.
- Urodynamic tests. These measure bladder function, recording pressure, capacity and flow.
- Cystoscopy. This involves an injection of a cystoscope via the urethra to inspect the bladder and urethra for abnormalities.
Most of the tests for incontinence are non-invasive and painless and don’t require any surgery, with little or no necessary preparation. Some tests may cause discomfort, while others require a full bladder, and most are painless and quick. Local anesthesia is typically used to reduce the discomfort of procedures like cystoscopy and other minimally invasive procedures.
What Can I Expect During and after Treatment?
 Most women have gradual symptoms and can recover with medication. Each of the many different treatments for urinary incontinence has different effects before, during and after the procedure. Non-surgical treatments require little or no recovery time. In contrast, surgical treatments like ovarian cyst removal may include a short rest and recovery time.
Most women have gradual symptoms and can recover with medication. Each of the many different treatments for urinary incontinence has different effects before, during and after the procedure. Non-surgical treatments require little or no recovery time. In contrast, surgical treatments like ovarian cyst removal may include a short rest and recovery time.
You see significant improvement in your symptoms, whichever route your doctor recommends.
Non-surgical treatments include:
- Pelvic floor exercises
- Bladder training
- Medications, such as anticholinergics, Botox or estrogen
Most surgical options are minimally invasive and take anywhere from 30 to 60 minutes, allowing you to return home quickly. You can expect mild discomfort or soreness, for which over-the-counter pain medications are sufficient. There are risks of infection or bleeding, but these are minimal with experienced specialists like Dr Cohen.
Surgical options for various types of incontinence, usually performed laparoscopically, include:
- Colposuspension
- Sling surgery
- Vaginal mesh surgery
Contact Cohen Medical Practice (CMP) for an appointment to take care of your stress incontinence and learn what causes the various other types of incontinence.

