What Is Premenstrual Syndrome?
Premenstrual syndrome, more commonly known as PMS, is a condition that many women go through before their monthly menstrual cycle. In the days leading up to your period, you may experience different symptoms that are physical, emotional or behavioral. It happens after the ovulation phase and is linked with hormonal imbalances in the cycle.
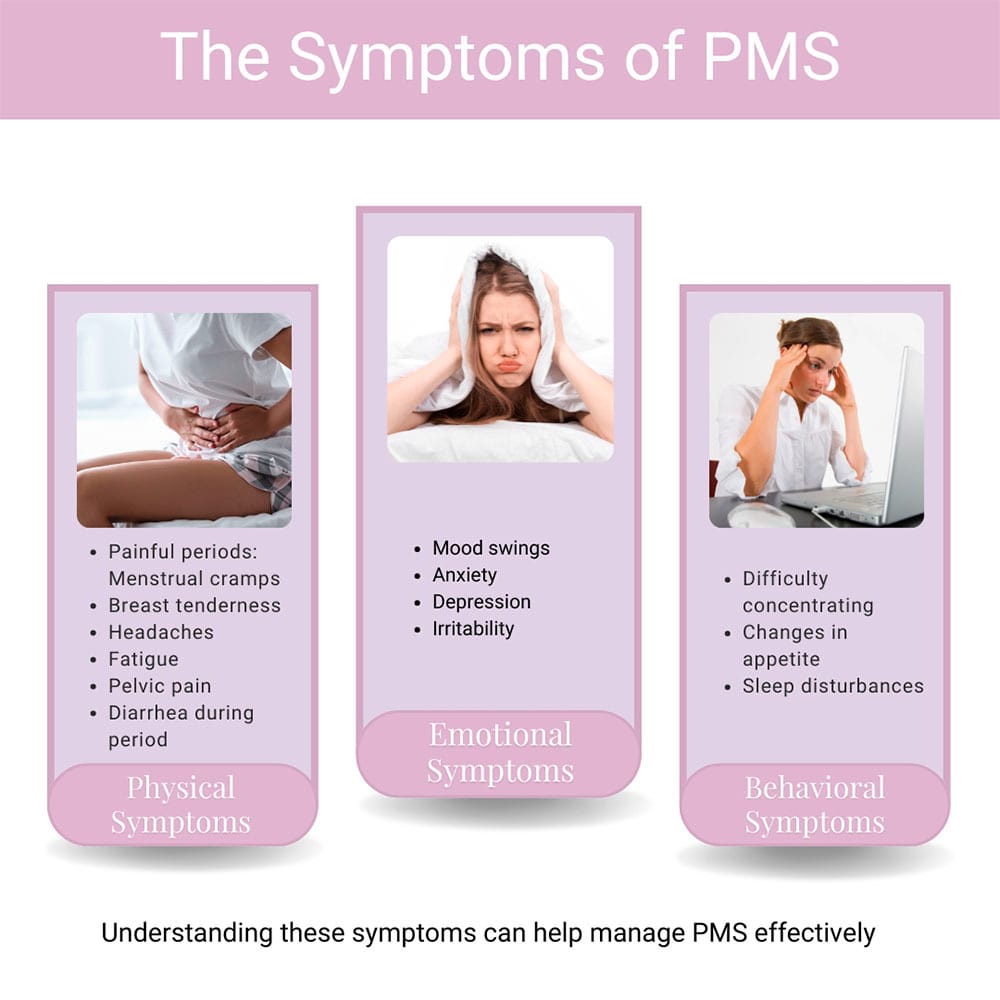
The symptoms of PMS may include:
- Physical symptoms, painful periods with things like breast tenderness, headache, fatigue, menstrual cramps before period, diarrhea during period and pelvic pain
- Emotional symptoms, such as mood swings, anxiety, depression and irritability
- Behavioral symptoms that sometimes show up as problems in concentration, changes in appetite and sleep issues
Women are affected by PMS differently, and the severity of symptoms varies from one woman to another. Pelvic pain in PMS contributes to pain during intercourse causing vaginal pain in some women. A condition called adenomyosis, where endometrial tissue grows into the uterine wall, worsens the symptoms of PMS making it more severe in some cases.
Untreated PMS leads to long-term stress, reducing your energy to deal with daily-life issues. Hormonal changes that are linked with PMS may also trigger other medical problems like migraines, urinary incontinence and irritable bowel syndrome. Find the most accurate diagnoses and effective treatment for PMS and other gynecological conditions at Cohen Medical Practice (CMP) in Midtown NYC.
What Do I Need to Know about Dysmenorrhea?
While the definition of PMS covers the gambit of premenstrual disorders, dysmenorrhea refers to painful menstrual cramps and extreme discomfort in the lower abdomen. It happens when your uterus contracts to shed its lining. You start getting painful period cramps before your periods and it gets better after a few days. Dysmenorrhea is of two types: primary and secondary.
Primary dysmenorrhea occurs without any medical issues. It’s usually caused when prostaglandins are released, which causes the uterus to contract and shed its lining.
Secondary dysmenorrhea is caused by other medical conditions, such as:
Intrauterine devices (IUDs) may also cause increased cramping and discomfort. The pain in this type of PMS starts earlier in the cycle and lasts longer than primary symptoms, creating cramps after period pain.
Common symptoms may include:
- Fatigue
- Headaches
- Nauseous feeling
- Vomiting
- Diarrhea
- Severe lower abdominal pain
- Severe cramps after period
- Severe cramps before period
How Is Dysmenorrhea Diagnosed?
Diagnosing a condition like dysmenorrhea involves a detailed evaluation to mark the underlying cause of the menstrual cramps. Your CMP doctor asks you about the duration and severity of your cramps and the history of your periods.
The next steps in the diagnostic process include:
- Pelvic exam
- Ultrasound
- Hysteroscopy
- Endometrial biopsy
- Blood tests
Depending on your diagnosis, your doctor develops a treatment plan designed to target your specific symptoms and provide you with a plan to move forward without the side effects. Dr. Cohen doesn’t believe that your monthly menstrual cycle needs to be so painful and disruptive.
How Can I Manage My Menstrual Cramps?
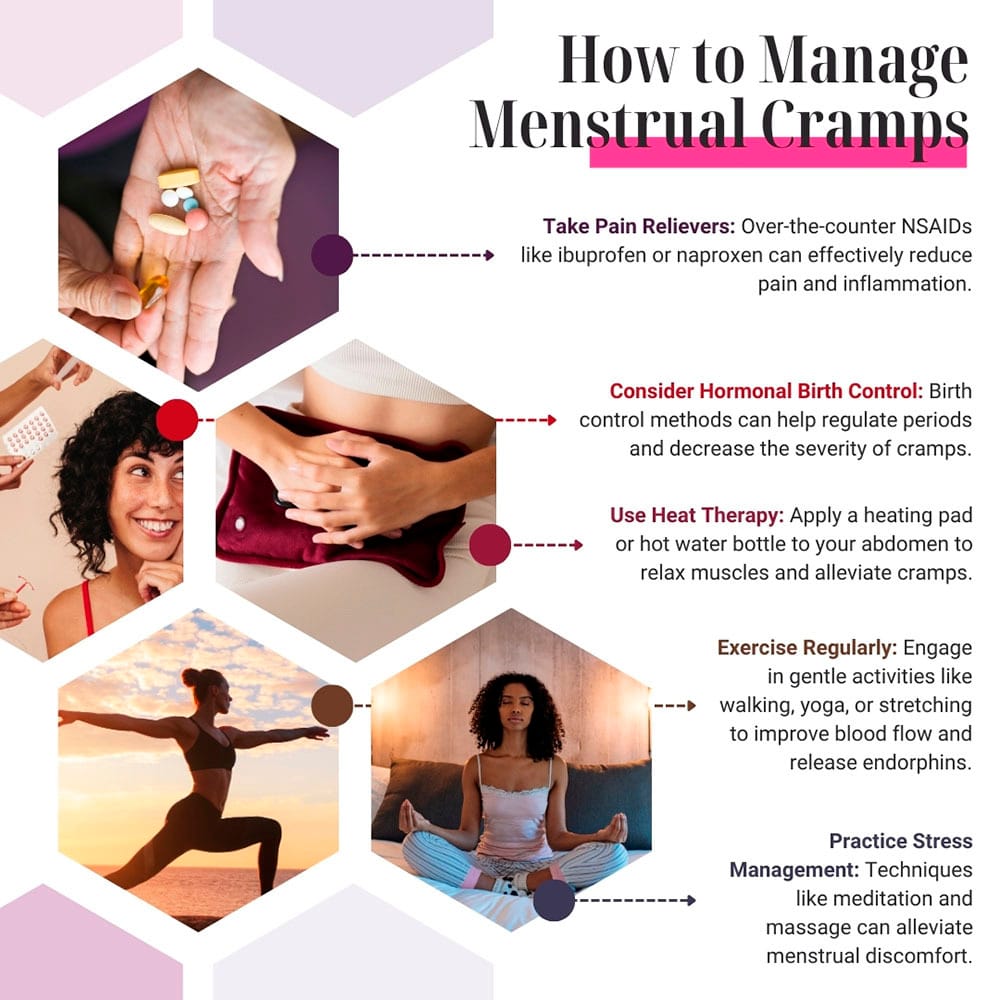
You can manage period cramps by combining various home remedies, lifestyle changes and medical treatments. Your CMP doctor may recommend non-steroidal anti-inflammatory drugs like ibuprofen or naproxen to reduce cramps. Opioids may be prescribed to reduce severe cramps.
Other treatment options may include:
- Using birth control medicines, patches, and hormonal IUDs, which also help in regulating periods and reducing pain
- Applying a heating pad or water bottle that may reduce your cramps and abdominal pain as it relaxes muscles
- Exercising regularly to improve blood flow and reduce cramps
- Eating a well-balanced diet and reducing caffeine, salt and alcohol
- Undergoing a laparoscopy procedure to treat conditions like PID and endometriosis
- Getting a D&C that may be recommended if abnormal uterine conditions are the cause of pain
- Doing yoga, meditation and counseling to help you manage stress and improve your overall well-being
- Finding relief through acupuncture, which helps balance the body’s energy
Often, women get diarrhea during periods, which can occur due to different factors related to hormonal changes and hidden medical conditions. If prostaglandins increase during menstruation, it impacts the gastrointestinal tract, which leads to diarrhea. Changes in estrogen and progesterone during your periods also impact bowel movements.
Other causes may include:
- Changes in diet
- Stress and anxiety
- Other medical conditions
What Can I Do to Treat Diarrhea during My Periods?
A balanced diet that’s rich in fruits, vegetables and fiber may be the surest way to regulate your bowel movements during your periods. Avoid foods that trigger diarrhea such as alcohol, spicy food, high-fat food and caffeine.
Follow your doctor’s orders, which may include:
- Staying hydrated
- Taking all prescribed medication
- Following hormonal treatments
- Managing your stress
Additionally, to reduce your PMS symptoms, eat foods high in calcium and magnesium such as nuts, seeds and whole grains. Get enough sleep every night and quit unhealthy habits like smoking, drinking and being sedentary that contribute to stress.
You can’t afford to lose energy. Treating dysmenorrhea helps you maintain your productivity and energy levels at work and in your relationships. If you’re tired of menstrual cramps and mood swings because of your PMS, then don’t ignore it. Contact Cohen Medical Practice (CMP) before your next cycle begins.

