What Is Rectocele?
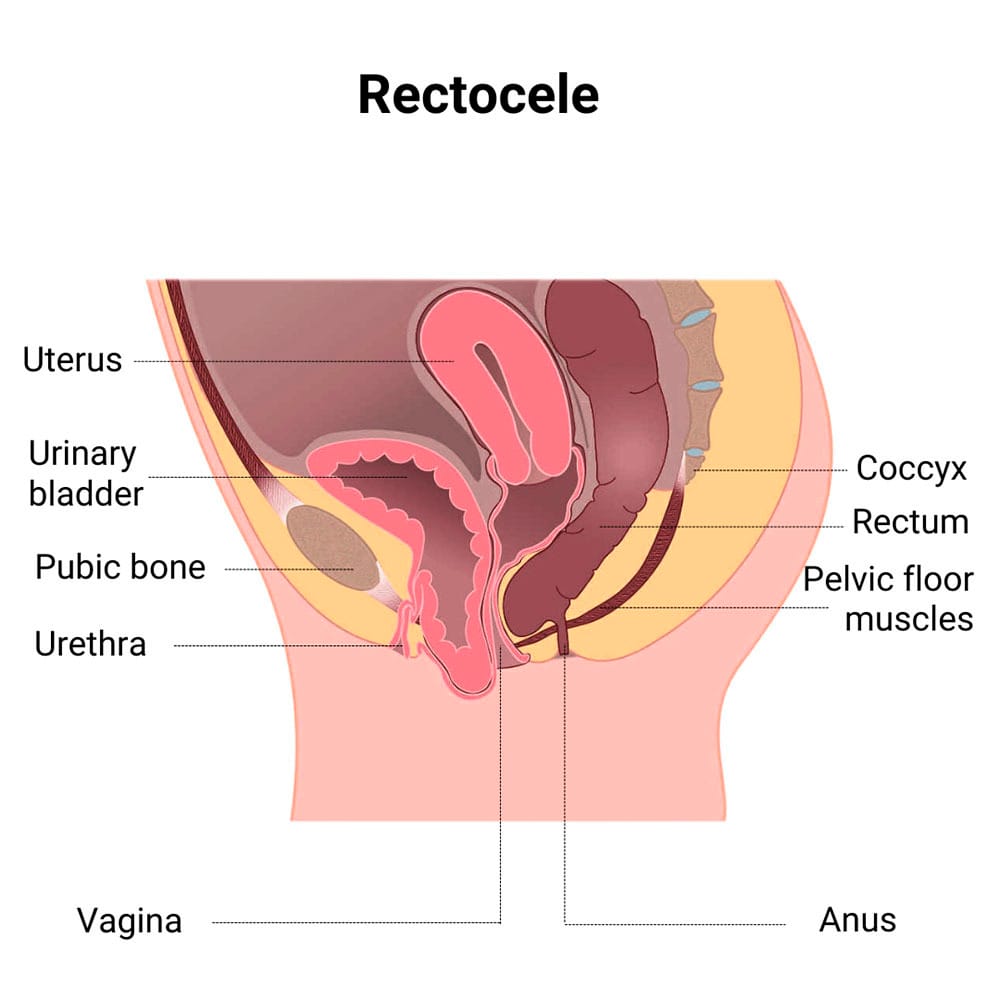 Rectocele, also called posterior prolapse, is a condition that occurs when the wall between your rectum and vagina weakens, causing your rectum to bulge into your vaginal canal. This happens when the tissues connecting your pelvic organs become stretched due to childbirth, aging or ongoing pressure on your pelvic floor.
Rectocele, also called posterior prolapse, is a condition that occurs when the wall between your rectum and vagina weakens, causing your rectum to bulge into your vaginal canal. This happens when the tissues connecting your pelvic organs become stretched due to childbirth, aging or ongoing pressure on your pelvic floor.
While rectocele and cystocele are both forms of pelvic organ prolapse, they differ because cystocele specifically affects the bladder rather than the rectum.
Whether you are experiencing pelvic pain, rectal pain or any other types of gynecological conditions, Dr. Felix Cohen, a board-certified obstetrician and gynecologist offers feminine health solutions in a comfortable and supportive environment at Cohen Medical Practice (CMP) in Midtown NYC.
What Are the Symptoms of Rectocele?
If you have a rectocele, you might find it challenging to fully empty your bowels. You may need to push more than usual or even have to press on your vaginal wall to help with bowel movements. You may notice a constant feeling of rectal pressure in your pelvic area. This sensation can get worse throughout the day.
While it is possible that you may not experience any symptoms from a rectocele, when you do, it’s usually very uncomfortable and may include:
- A bulge in your vaginal wall, which can protrude through the vaginal opening
- Lower back pain due to the changes in your posture as you adjust to the condition
- Pain during sex because of rectal pressure in the vaginal area
You may find yourself struggling with chronic constipation without proper support for the rectum when moving your bowels can be difficult. If you have a rectocele along with a bladder prolapse, you may also experience urinary incontinence and feel an increased urge to urinate or deal with leakage.
What Causes a Rectocele?
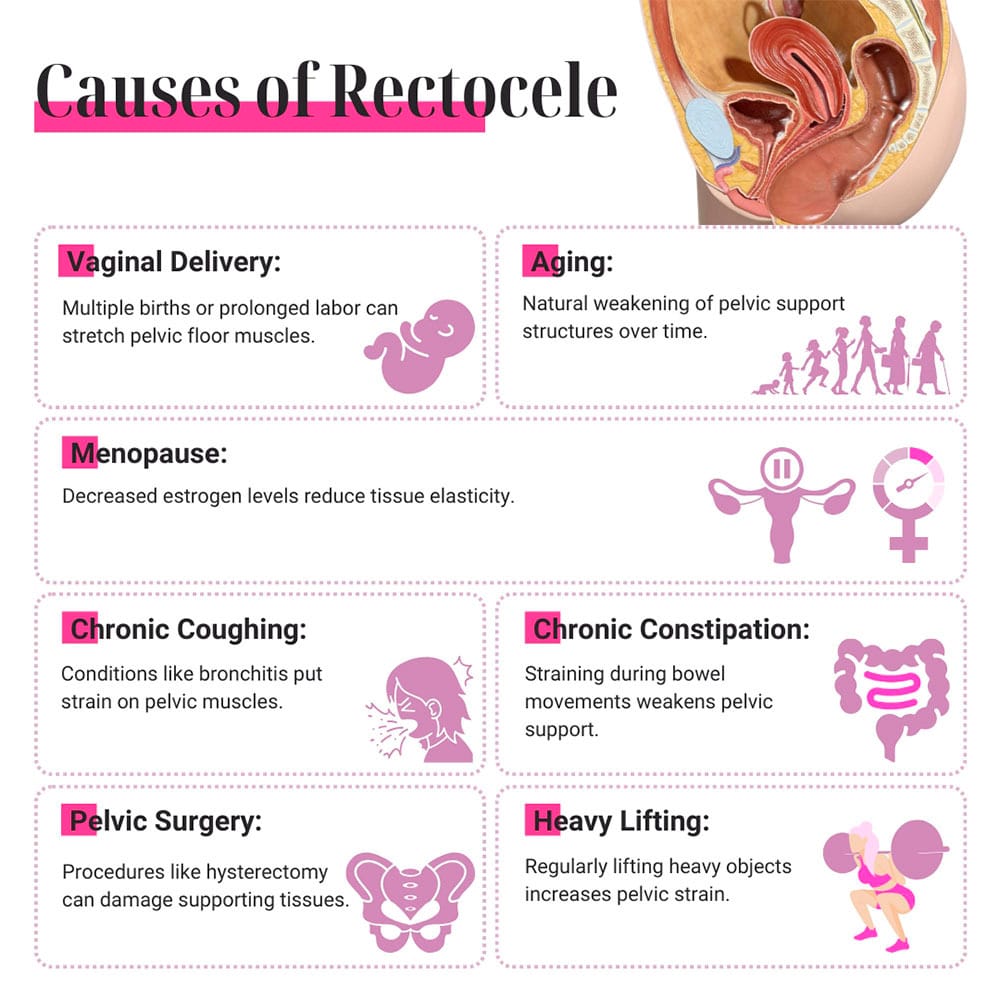
Rectocele can be caused due to vaginal delivery, especially when you’ve had multiple births that stretch and weaken your pelvic floor. Prolonged labor and having larger babies further stretch these muscles, which reduces support for your vaginal wall and increases your risk of developing a rectocele.
Several other factors that contribute to rectocele development include:
- Aging. Your pelvic floor gets weaker over time and loses its strength. Menopause brings further changes in your body, such as decreased estrogen levels, which can contribute to the development of a posterior prolapse.
- Bronchitis. If you have a constant cough from conditions like asthma, smoking, bronchitis or other respiratory diseases, it places a continuous strain on your pelvic floor and increases the risk for rectocele.
- Chronic constipation. If you often push hard to pass stools, it can gradually weaken your pelvic floor muscles.
If you had surgeries on your pelvic organs, such as a hysterectomy, it may have harmed the tissues in your pelvic floor and raised the risk of a rectocele. Daily activities, like lifting heavy objects consistently at work or in the gym, can also place extra strain on your pelvic floor muscles and make you more susceptible to a rectocele.
How Is Rectocele Diagnosed?
Your diagnostic process starts with a conversation with your doctor about your symptoms, medical history, any surgeries, childbirth experiences and other factors that could have weakened your pelvic muscles.
Your CMP doctor also conducts a physical exam and may ask you to bear down as if you’re having a bowel movement, while he feels inside your pelvis. This helps him see whether the vaginal wall is bulging due to rectal pressure or any secondary prolapses.
Other diagnostic tests may include:
- Pelvic ultrasound
- Magnetic resonance imaging (MRI)
- Defecography
- Cystoscopy
How Do You Treat a Rectocele?
Posterior prolapse has a range of surgical and non-surgical treatment options available to you depending on how mild or severe your rectocele is. Mild cases can be treated with a consistent regimen of Kegel exercises, which strengthen the muscles that support your pelvic organs. If you regularly perform these exercises, your muscle tone and support for your vaginal and rectal walls improves.
If your rectocele is at a moderate level, then a vaginal pessary may be recommended by your doctor. This is a safe device that can be used long-term to hold your vaginal wall in place and commonly used to treat pelvic organ prolapses. If non-surgical methods aren’t enough to resolve your symptoms, however, surgery for rectocele treatments might be an option for you.
Rectocele repair includes:
- Strengthening the wall that’s been weakened between your rectum and your vagina
- Making a small incision in the back of your vaginal cavity
- Suturing the layers of tissue under the wall so that the area is tightened and reinforced
What Is Recovery from Posterior Prolapse Treatment Like?
Recovery from posterior prolapse surgery takes between three and six weeks, during which time you must avoid sex and take stool softeners to prevent constipation. Your CMP doctor may also recommend that you refrain from heavy lifting and only slowly return to your normal level of activities until you’re fully healed to prevent further prolapse.
For more information about rectocele and other types of gynecological issues you may be having, make an appointment with Dr. Cohen by contacting Cohen Medical Practice (CMP) in Midtown NYC at the first signs of prolapse or vaginal discomfort. The sooner you receive treatment, the easier your recovery from posterior prolapse becomes.

