What Is a Cystocele?
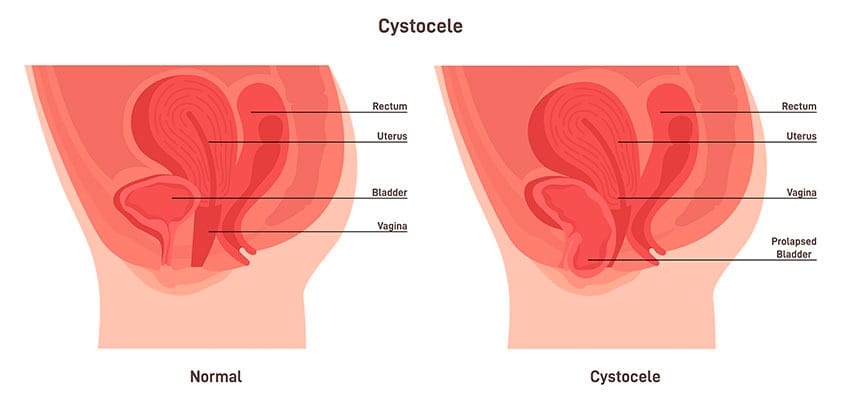
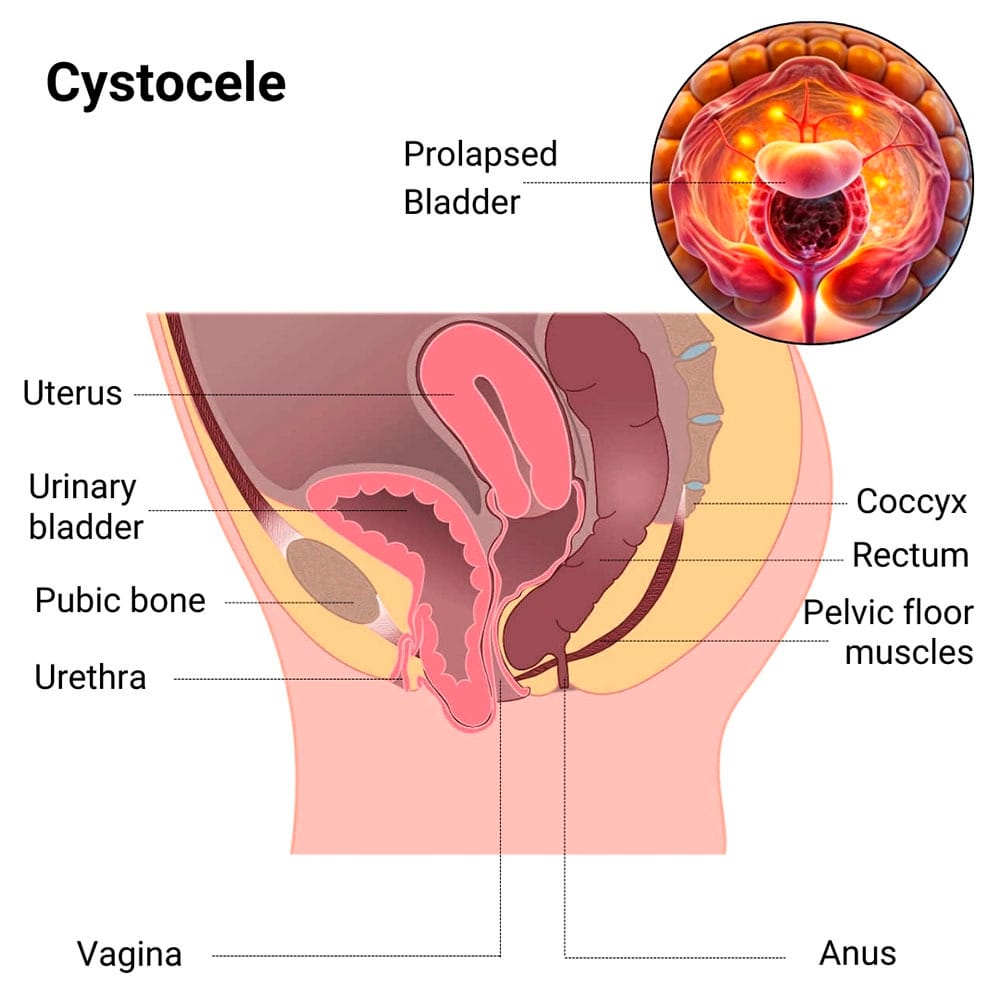 A cystocele, also called anterior prolapse, happens when the tissue that supports your bladder and vaginal wall weakens or stretches. It’s a type of pelvic uterine prolapse that’s common among women, especially after childbirth or menopause. This causes your bladder to drop into the vagina, which leads to a bulging sensation along with urinary or pelvic symptoms.
A cystocele, also called anterior prolapse, happens when the tissue that supports your bladder and vaginal wall weakens or stretches. It’s a type of pelvic uterine prolapse that’s common among women, especially after childbirth or menopause. This causes your bladder to drop into the vagina, which leads to a bulging sensation along with urinary or pelvic symptoms.
Your bladder may shift downward and press against the front wall of the vagina. This creates bladder infections and anterior prolapse. It’s a common condition that can cause you discomfort and urinary problems, but with the right care and treatment you can fully resolve the issue.
Whether the prolapse is mild or severe, find relief from rectocele and cystocele at Cohen Medical Practice (CMP). Dr. Felix Cohen, a board certified obstetrician and gynecologist, specializes in female health and reproductive issues, and offers advanced gynecological services ranging from ectopic pregnancies to fertility treatments and sexually transmitted diseases.
What Are the Causes and Risk Factors for Developing a Cystocele?
Vaginal childbirth is one of the most common causes of cystocele. Your pelvic muscles and supportive tissues become stretched during labor and delivery. This weakens the muscles and ligaments that normally hold your bladder in place. You can even have a higher risk if you go through multiple deliveries or experienced complications during childbirth.
Other factors that contribute to the development of a cystocele include:
- Being obese, as the extra weight can weaken your pelvic muscles and their ability to support your bladder
- Having chronic constipation or a persistent cough, which increases the pressure on your pelvic region, stretching and weakening the supportive tissues
- Doing heavy lifting frequently, whether through work or during your exercise routine
Your pelvic tissues also naturally lose strength and elasticity as you age. During menopause when your estrogen levels drop, it stops keeping your vaginal tissues strong and healthy.
What Are the Symptoms of a Cystocele?
Your pelvic area might feel heavy or pressured when cystocele develops, which often increases after you stand for long periods, carry heavy objects or are physically active. It usually becomes uncomfortable or even painful as the day progresses.
Another sign you may notice is a bulge or protrusion in your vagina, which is caused by your bladder dropping into the vaginal canal. This bulge may even extend outside your vaginal opening and become visible.
Other symptoms of an anterior prolapse you might experience include:
- Urinary incontinence because your bladder’s new position affects its function, feeling your bladder isn’t emptying fully and leaking urine especially when you sneeze, cough or laugh
- Bladder infections that may occur from your urethra being more exposed to outside bacteria
- Abnormal uterine bleeding because of the excessive pressure on your pelvic organs
- Pain during sex because the bulge pressing into your vaginal wall causes pressure that makes intercourse less enjoyable and uncomfortable
- Difficulty with bowel movements or experiencing constipation as the prolapse presses on your rectum, making it harder to pass stool comfortably
You could be more prone to urinary tract infections since your bladder may not be emptying completely. This also creates an environment where bacteria can grow and leads to frequent infections when urine remains in the bladder for too long.
How is a Cystocele Diagnosed?
Early stages of anterior prolapse aren’t always obvious during your annual gynecological exam, so your CMP doctor relies on your explanation of your symptoms. Having repeated bladder infections may tip him off to look for cystocele as well. During your visit, a pelvic examination is done during which you may be asked to cough or bear down so your doctor can assess the degree of prolapse.
He also looks for signs of rectocele and cystocele occurring together, which may require more aggressive treatments. Imaging tests with contrast dye may be needed to get a more detailed view of your pelvic organs.
Other diagnostic methods may include:
- Cystoscopy
- Sonogram
- Urodynamic testing
What Treatments Are Available for a Cystocele?
There are several treatments available that depend on how severe your condition is. Your CMP doctor may suggest using a pessary, which is a small removable device that’s placed inside your vagina for bladder lift and preventing it from bulging. You also may be guided to lose weight to reduce the pressure on your vaginal wall.
Pelvic floor exercises, called Kegel exercises, are one of the most effective non-surgical options. Your NYC physician may recommend physical therapy to guide you in how to do these exercises correctly to get the most benefit. If your cystocele is more advanced or non-surgical options haven’t relieved your symptoms, cystocele surgery may be the next step to restore your bladder’s position and strengthen weakened tissues.
Surgical treatments may include:
- Pelvic floor reconstruction
- Abdominal repair surgery
- Bladder lift
- Vaginal vault suspension
- Uterine suspension
- Hysterectomy
Recovery time from anterior prolapse surgical treatments depends on your overall health and how severe the prolapse. While you may need prescription pain relief at first, your doctor quickly moves you to over-the-counter pain medicine while you continue to rest and recover for the next couple weeks.
If you’re noticing pelvic pressure or discomfort from conditions like anterior or posterior prolapse, contact Cohen Medical Practice (CMP) as soon as possible. The earlier you receive treatment for the condition, the easier the treatment and the less recovery time from anterior prolapse procedures you need.

