What Is a Prolapsed Bladder?
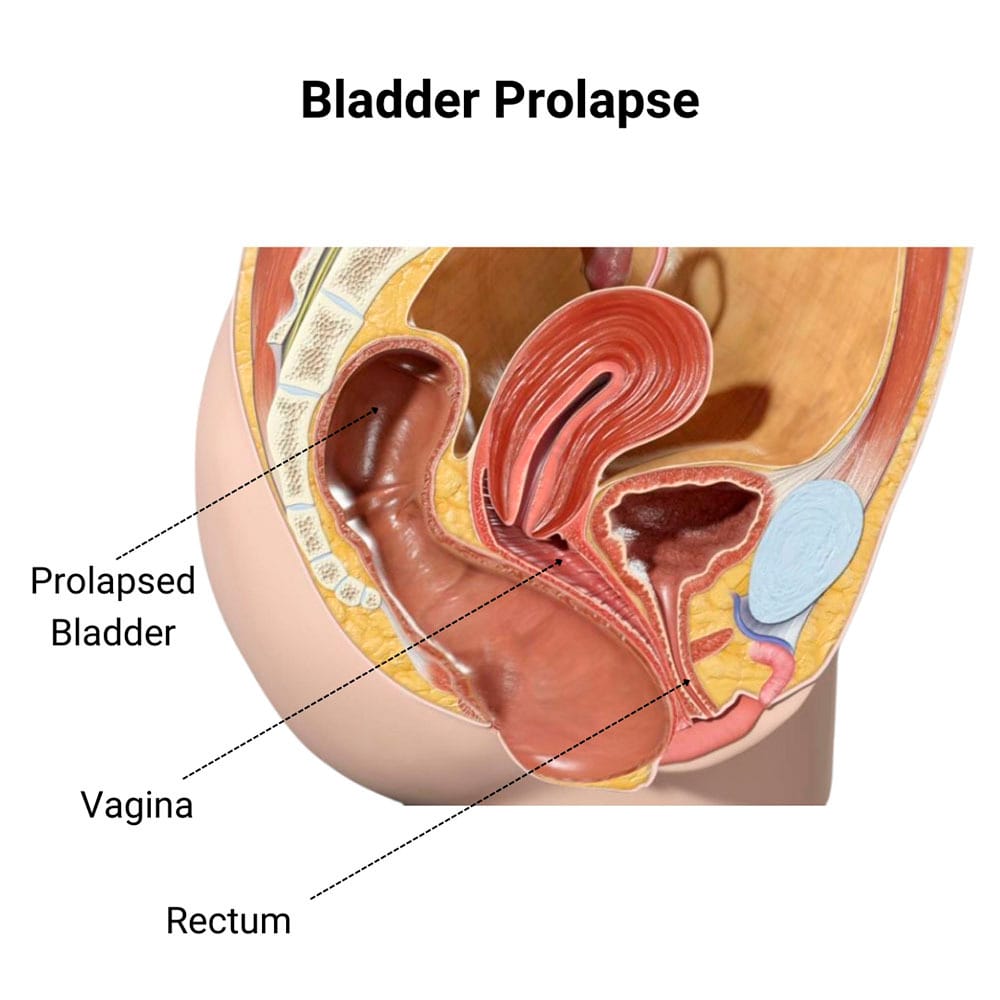 A prolapsed bladder occurs when the muscles and ligaments holding the bladder in place become weakened and can’t hold the bladder in its proper place. These fragile tissues then cause the bladder to move downward, encroaching on the vagina.
A prolapsed bladder occurs when the muscles and ligaments holding the bladder in place become weakened and can’t hold the bladder in its proper place. These fragile tissues then cause the bladder to move downward, encroaching on the vagina.
A prolapsed bladder is a condition called cystocele, which is a pelvic organ prolapse that’s also known as a:
- Dropped bladder
- Fallen bladder
- Herniated bladder
At its worst, prolapse bladder pain happens and causes the bladder to impede the vaginal opening. A bladder prolapse is a fairly common occurrence, with up to 50 percent of women having some sort of sagging of the bladder.
When mild, you may not even know you have a prolapse if there are no symptoms. When it becomes severe, it can cause a multitude of physical problems. If you believe you may have a prolapsed bladder, Dr. Felix Cohen at Cohen Medical Practice (CMP) New York offers an extensive line of diagnostic techniques and treatment plans for a prolapsed bladder and other gynecological conditions.
What Are the Symptoms of a Prolapsed Bladder?
The manifestations of a prolapsed bladder depend on the stage of the cystocele. The signs of a dropped bladder can also change for a variety of reasons. Premenopausal women may have more pain during their period, while some may notice that having intercourse is uncomfortable. Many women with a stage one prolapse may have no noticeable signs.
Some of the more common symptoms include:
- Frequent urinary tract infections
- A feeling of fullness or pain in the groin
- Urinating more often than usual
- Feeling something protruding from your vagina
When symptoms are similar to other conditions, you need to have an experienced gynecologist provide you with the most accurate diagnosis to receive the proper treatment for your pain and discomfort.
How Is Bladder Prolapse Diagnosed?
When you see your CMP physician, he first performs a pelvic examination to determine the extent of the prolapse. You may be asked to bear down during this physical exam to give him an idea of how far it drops.
For more precise information, he relies on other types of tests as well that may include:
- MRI to see exactly where all your organs are setting at the time
- Urodynamic testing to determine how well your bladder can hold and release urine
- Cystoscopy, which uses a small camera inserted into the bladder through the urethra to look for abnormalities
These tests also allow your physician to determine what stage of prolapsed bladder you’re experiencing. Cystocele has three basic stages. And although they may overlap in some of the symptoms, your physician uses these measurements to tell how much your bladder has dropped.
The stages and their associated characteristics include:
- Stage 1, which is considered mild, when your bladder has dropped only slightly, and you haven’t shown any signs or symptoms. This slight bladder drop may have been noticed during your annual gynecological exam.
- Stage 2 is an intermediate bladder prolapse when it’s dropped into the vagina, making it bulge when you’re active or on the toilet. You’ll experience mild symptoms and bladder problems during this stage.
- Stage 3 is severe and requires mediation because by this time, your bladder has fallen enough to block and bulge out of your vagina, making it nearly impossible for sex or to insert a tampon.
What Are the Treatment Options?
Treatments for cystocele vary depending on what stage it’s in. When it’s mild in stage one, you may be able to address the prolapse with lifestyle changes and physical therapy. When it’s in the last stage, it may be necessary to have bladder prolapse surgery to repair or replace the muscles and tendons that hold your bladder in place.
If you have prolapsed bladder pain, incontinence or other bladder problems, treatment options that are less invasive than surgery may work for you and include:
- Kegel exercises to help strengthen pelvic muscles
- Losing weight and maintaining an appropriate weight to reduce the pressure on your bladder
- Estrogen replacement therapy, especially vital for women in menopause who experience thinning of the vaginal tissues that lead to conditions like prolapsed bladder, other forms of anterior prolapse and posterior prolapse.
If your symptoms are alleviated by one or more of these methods, you also should avoid heavy lifting at work or in the gym and straining when moving your bowels. This could result in damaging your ligaments and muscles again. If you have a moderate to severe prolapsed bladder, you may need bladder prolapse surgery to eliminate the problem.
What Can I Expect during My Prolapsed Bladder Surgery Recovery?
During bladder prolapse surgery, known as anterior colporrhaphy, your doctor tightens the muscles that keep the bladder in place. This is normally done on an outpatient basis and complete recovery typically lasts a couple months.
While you can return to your normal activities in a week or so, you also want to avoid things like:
- Doing any heavy lifting
- Developing a cold that leads to coughing
- Smoking that also causes coughing and slows healing
- Constipation so you don’t have to strain
For prolapsed bladder surgery recovery, your doctor may provide stool softeners or cough medicine to help you avoid unnecessary pain and re-damage the tender vaginal tissue. If you need to see a physician for symptoms related to a fallen bladder or other gynecological issues, contact Cohen Medical Practice (CMP) as soon as possible.

